There are many questions asked about diets for specific diseases. Here are the most diseases and diets:
Acne : low fat
Acute gastroenteritis : clear liquid
Acute glomerulonephritis : low Natrium, low Protein
Addison disease : high Natrium, Low kalium
Anemia - iron deficiency : high iron
Anemia - pernicious : high protein, vitamin B
Anemia – sickle cell : high fluid
Angina pectoris : low cholesterol
Arthritis – gout : purine restricted
Attention Deficit Hyperactivity Disorder (ADHD) : finger foods
Bipolar disorder : finger foods
Burn : high calorie, high protin
Celiac's disease : gluten free
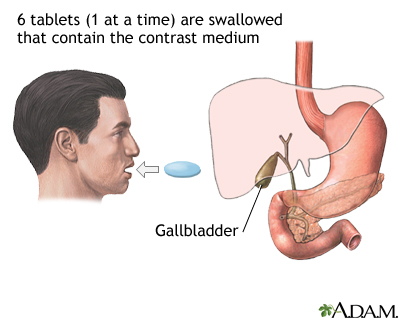
Cholecystitis : high protein, high carbohydrate, low fat
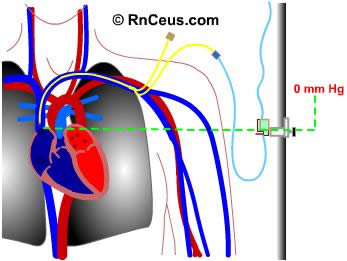
Congestive heart failure : low natrium, low cholesterol
Congestive heart failure : low natrium, low cholesterol
Cretinism : high protein, high calcium
Crohn disease : high protein, high carbohydrate, low fat
Cushing disease : high kalium, low natrium
Cystic fibrosis : high calorie, high natrium
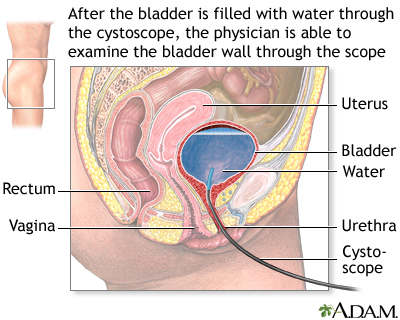
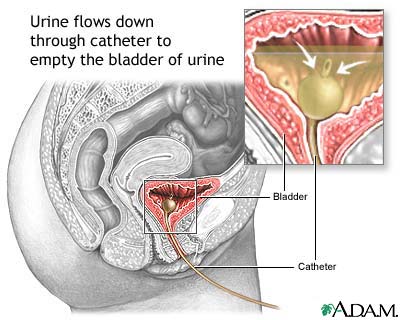
Cystitis : acid ash (for alkaline stones) and alkaline ash( for acid stones)
Decubitus ulcer : high protein, high vitamin C
Diabetes mellitus : well balanced diet
Diarrhea : high kalium, high natrium
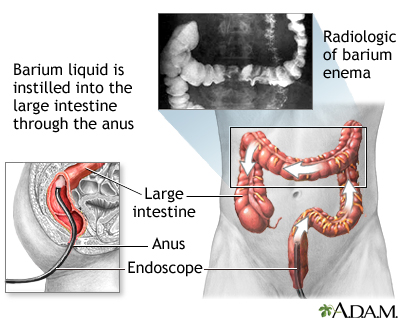
Diverticulitis : low residue
Diverticulosis : high residue with no seeds
Dumping syndrome : high fat, high protein, dry food
Hepatic encephalopathy : low protein
Hepatitis : hight protein, high calorie
Hirschsprung disease : high calorie, low residue, high protein
Hyperparathyroidism : low calcium
Hypertension : salt restricted
Hyperthyroidism : high calorie, high protein
Hypoparathyroidism : high calcium, low phosphorus
Hypthyroidism : low calorie, low cholesterol, low saturated fat
Kawasakis' disease : clear liquid
Liver cirrhosis : low protein
Meniere's disease : low natrium
Myocardial infarction : low fat, low cholesterol, low natrium
Nephritic syndrome : low natrium, high protein, high calorie
Osteoporosis : high calcium, high vitamin D
Pancreatitis : low fat
Peptic ulcer : high fat, high carbohydrate, low protein
Phenylketonuria : low protein/phenylalanine
Pregnancy induced hypertension : high protein
Renal colic : low sodium, low protein
Renal failure – acute : low protein, high carbohydrate, low natrium (oliguric phase), high protein, high calorie, restricted fluid (diuretic phase)
Renal failure – chronic : low protein, low natrium, low kalium
Tonsillitis : clear liquid
MAJOR DIETARY SOURCES:
CARBOHYDRATE
- Bread
- Cereal
- Crackers
- Corn
- Potatoes
PROTEIN
FAT SOURCE
- Margarine
- Avocado
- Nuts
- Olives
- Peanut
- Mayonnaise
Read more...